Introduction to Telemedicine
Telemedicine, a transformative approach in healthcare, employs telecommunications technology to provide medical services and consultations remotely. The concept originated in the 1960s with the use of telecommunication tools to support healthcare delivery in remote areas. Over the years, telemedicine has evolved significantly, driven by advancements in technology and the changing needs of healthcare systems.
The crux of telemedicine involves the exchange of medical information via electronic communication, enabling patients to receive care without the necessity of in-person visits. This is executed through various forms, including video consultations, remote patient monitoring, and mobile health apps. These technologies facilitate a comprehensive range of services such as diagnosis, treatment, follow-up consultations, and patient education.
Telemedicine’s importance has surged in recent years due to its ability to enhance accessibility to healthcare services, particularly for individuals in rural or underserved regions. The COVID-19 pandemic has further accelerated the adoption of telemedicine. With lockdowns and restrictions limiting physical interactions, telemedicine emerged as a critical solution to continue providing essential healthcare services. According to a study published in JAMA Network Open, telemedicine usage saw a 4000% increase during the early months of the pandemic, underscoring its vital role in maintaining healthcare continuity.
Statistics vividly illustrate the growth and effectiveness of telemedicine. The American Medical Association reported that in 2016, only 15% of physicians in the U.S. engaged in telemedicine. By 2021, this number leapt to 79%, highlighting a rapid and robust adoption. Moreover, research has shown that telemedicine not only increases access to care but also improves patient outcomes, demonstrating efficacy in managing chronic conditions, mental health issues, and acute medical situations.
As technology continues to advance and the healthcare landscape evolves, telemedicine is poised to remain a pivotal component of healthcare delivery. Its capacity to overcome geographical barriers and provide timely, efficient, and patient-centered care underscores its indispensable role in contemporary healthcare systems.
Benefits and Advantages of Telemedicine
Telemedicine stands as a transformative advancement in the healthcare industry, delivering a multitude of benefits for both patients and healthcare providers. One of the primary advantages is the improved access to healthcare services, particularly for individuals residing in rural or underserved areas. Through telemedicine, patients who may have previously faced significant barriers to receiving care can now consult with medical professionals without the need for extensive travel. This enhanced access is crucial in addressing healthcare disparities and ensuring that every individual receives timely medical interventions.
Convenience and time savings are also significant benefits of telemedicine. Patients can schedule appointments based on their availability, reducing the need to take time off work or arrange for childcare. The elimination of travel time is particularly beneficial for those with mobility issues or chronic conditions. Moreover, telemedicine facilitates ongoing management of chronic diseases by allowing patients to have regular check-ins with their healthcare providers, leading to better health outcomes and a higher quality of life.
From a financial perspective, telemedicine has the potential to reduce healthcare costs significantly. By minimizing the need for hospital visits and reducing the frequency of emergency room admissions, telemedicine can lower overall healthcare expenditures. Additionally, it allows healthcare providers to allocate their resources more efficiently, ultimately contributing to a more sustainable healthcare system.
Technological advancements have played a pivotal role in making telemedicine more efficient and reliable. High-resolution video conferencing, secure electronic health records (EHRs), and advanced diagnostic tools ensure that patients receive the same level of care as they would during in-person visits. These technologies also enable healthcare professionals to collaborate more effectively, leading to faster diagnosis and treatment plans.
In summary, telemedicine offers substantial benefits that enhance patient care, promote equitable access to healthcare services, and contribute to cost savings. As technological innovations continue to advance, the reliability and effectiveness of telemedicine are expected to improve, further cementing its role in modern healthcare.
As telemedicine continues to evolve as a critical component of modern healthcare delivery, it faces several challenges and limitations that need to be addressed to optimize its potential. One significant challenge is the digital divide, which pertains to the disparity in access to reliable internet and digital devices among different populations. Rural areas, underserved communities, and low-income households often struggle with insufficient connectivity, impeding their ability to leverage telemedicine services effectively.
Moreover, concerns about data privacy and security are paramount. The transmission of personal health information over digital platforms raises the risk of data breaches and cyberattacks. Ensuring robust encryption techniques and adherence to regulatory standards like HIPAA (Health Insurance Portability and Accountability Act) becomes essential to protect patient information.
The current regulatory framework for telemedicine also poses its own set of challenges. The absence of uniform telehealth regulations across different states and countries leads to inconsistencies in practice and reimbursement policies. This can act as a deterrent for healthcare providers who may already be reluctant to adopt telemedicine due to concerns about training, integration with existing systems, and workflow disruption.
There is also inherent resistance from both healthcare providers and patients. Some healthcare professionals may be skeptical about the efficacy of virtual consultations compared to traditional in-person visits. They often worry about the potential limitations in diagnosing and treating conditions remotely, such as the inability to perform physical examinations or conduct certain diagnostic tests. Patients, on the other hand, might be hesitant to trust virtual consultations, particularly older adults who may not be as comfortable with technology.
Despite these challenges, various initiatives and solutions are being implemented to bridge the gaps. Telehealth literacy programs are aimed at educating both providers and patients about the benefits and usage of telemedicine. Investments in broadband infrastructure seek to mitigate the digital divide, while advancements in encryption technologies aim to enhance data security. Regulatory bodies are increasingly working towards harmonizing telehealth guidelines to facilitate smoother adoption across different regions. These efforts highlight the ongoing commitment to overcoming the hurdles and maximizing the efficacy of telemedicine.
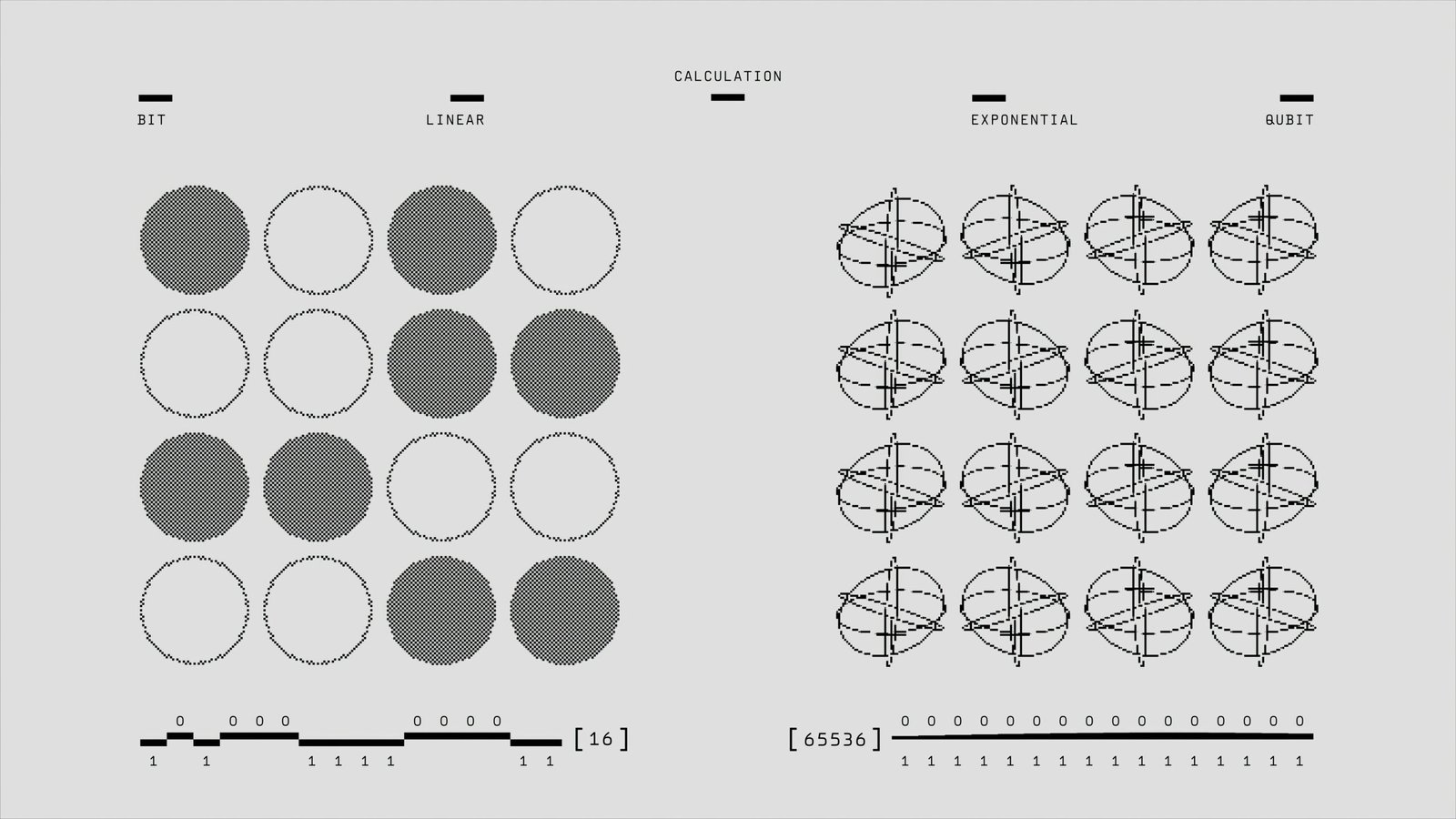
As we cast our eyes towards the future of telemedicine, the potential advancements and integrations poised to reshape remote healthcare are both vast and promising. The trajectory appears firmly aligned with the integration of sophisticated technologies, such as Artificial Intelligence (AI) and Machine Learning (ML), which are expected to revolutionize patient diagnosis, treatment plans, and personalized medicine. AI-driven algorithms can analyze vast datasets, providing healthcare practitioners with deeper insights and predictive analytics that could foresee health issues before they become critical.
Remote monitoring tools are another burgeoning trend within telemedicine. Wearable devices and Internet of Things (IoT) enabled health monitors can continuously track vital statistics, offering real-time data to healthcare providers. This seamless flow of information can support timely interventions and chronic disease management, significantly enhancing care quality and patient outcomes. The confluence of these technologies will propel telemedicine towards becoming an indispensable component of everyday healthcare.
Furthermore, the expansion of telemedicine services is expected to encompass more specialized fields. From dermatology to psychiatry, telehealth platforms are increasingly catering to niches within healthcare that have traditionally relied on in-person consultations. By removing geographical barriers, specialized care can become more accessible to under-served populations, thus democratizing healthcare.
The traditional healthcare landscape may witness a transformative shift towards a more patient-centered model. Telemedicine empowers patients, providing them with greater control over their health through seamless access to medical advice and continuous monitoring. This shift towards a more data-driven approach is expected to enhance patient engagement and compliance, resulting in better health outcomes and optimized resource allocation within healthcare systems.
Experts are optimistic about the long-term impact of telemedicine on healthcare delivery and public health. As per predictions by healthcare futurists, the next decade could see telemedicine evolving into a mainstream mode of healthcare delivery, playing a crucial role in epidemic response, rural health improvement, and overall health system efficiency. As these technologies mature, the future of telemedicine promises a paradigm where healthcare is efficient, accessible, and significantly more personalized.